The 2022 Global Specialty Lens Symposium (GSLS), presented by Contact Lens Spectrum, was held Jan. 19 to 22 at Bally’s in Las Vegas and, once again, it was a very successful forum for the most current clinical education pertaining to timely topics in specialty lens education. Against the backdrop of the pandemic, GSLS 2022 experienced an impressive attendance of more than 600 people from around the country—and the globe.
This year’s continuing education (CE) program included three workshops, eight general sessions, and 19 courses with an emphasis on myopia management, scleral lenses, management of the irregular cornea, dry eye, contact lens multifocals, and specialty lens practice management. In addition, there were more than 100 scientific posters, several free papers highlighting cutting-edge research, and almost 40 sponsored presentations, allowing attendees to learn about new specialty lens designs, technologies, and services being offered by industry.
The 2022 GSLS Education Committee is comprised of Jason J. Nichols, OD, MPH, PhD (chair); Karen DeLoss, OD (vice chair); Edward S. Bennett, OD, MSEd; Patrick Caroline; Lynette Johns, OD; and Eef van der Worp, BOptom, PhD.
MYOPIA, MYOPIA, MYOPIA
Myopia management was a popular topic at GSLS, highlighted by the general session “Myopia Control: Treatment Showdown 2.0,” moderated by Jeff Walline, OD, PhD, with an outstanding panel consisting of Pauline Cho, BOptom, MEd, PhD; Kate Gifford, PhD, BAppSci(Optom)Hons; Sally Dillehay OD, EdD; and Ashley Wallace-Tucker, OD. A series of seven cases were presented and each panel member argued for a different treatment option: orthokeratology (OK), soft multifocals (MF), myopia control glasses (MCG), and low-dose atropine (LDA). Then, the audience was polled as to what therapeutic option they believed to be indicated in that particular case. The cases and polling results are summarized in Table 1.
| CASE HISTORY | PRESENTER ARGUMENTS | POLL RESULTS |
|---|---|---|
| CASE 1: 2-year-old child already a moderate myope |
|
62% LDA22% MCG 11% OK 5% MF |
| CASE 2: 9-year-old boy, low (–1.75D) myope, does not like touching eye |
|
36% MCG 31% OK 22% LDA 11% MF |
| CASE 3: 11-year-old, OD: –1.00 –1.50 x 170; OD: –1.25 –1.25 x 010 |
|
62.5% OK 22% MCG 12.5% LDA 3% MF |
| CASE 4: 11-year-old male anisometropic; OD: +0.25 –0.50 x 180; OS: –2.25 –0.25 x 180 |
|
41.3% OK 34.7% MF 19.3% LDA 4.7% MCG |
| CASE 5: 6-year-old emmetropic male but should become myopic |
|
64.3% LDA 25.2% MCG 6.5% OK 4% MF |
| CASE 6: 10-year-old female; OD –1.75DS, OS: –1.50DS; patient likes wearing glasses; wants contact lenses for dance and softball only |
|
37.2% MF 27.7% OK 22.6% MCS 12.4% LDA |
| CASE 7: 12-year-old female; OD: –7.75DS. OS: –8.50DS, she is a competitive athlete |
|
69.4% MF 18.2% OK 6.2% LDA 6.2% MCG |
| OK, orthokeratology; MF, soft multifocals; MCG, myopia control glasses; LDA, low-dose atropine | ||
The presenters emphasized that all treatments can be effective. As the results showed in these cases, each method was preferred in, at minimum, one of the cases. Other outcomes gleaned from this session included:
- Lifestyle changes can be beneficial—in particular, less time on computers and cell phones and more time spent outside (i.e., “more green time and less screen time”).
- It does not appear that soft MF lenses are detrimental to athletes due to peripheral defocus and, in fact, the benefits to their quality of life are evident.
- For LDA, 0.05% is recommended although 0.025% can be used if glare and near problems are predicted. Glare is more likely to occur with those patients who have lighter skin, hair, iris color, etc. The Low-Concentration Atropine for Myopia Progression (LAMP) Study found that 0.01% was only half as effective as 0.05%.1
• Myopia Workshop
In their “Myopia Workshop: Moving Orthokeratology Forward in 2022” program, myopia management experts Patrick Caroline and Randy Kojima emphasized the need to use multiple modalities to handle the diversity of young progressive myopes, stating that to use just one would not be optimal. They said that this would be synonymous with only using one modality for controlling glaucoma. They also brought recent research to the forefront, including:
Slow Versus Fast Progressors Based upon the work of Rose et al,2 the Pacific University research group has concluded the following:
- Children who are low hyperopes, emmetropes, or low myopes should have their axial length monitored every six to 12 months.
- A six-month increase of axial length of less than 0.1mm would be slow myopia progressors (i.e., approximately ≤ –0.25D).
- A six-month increase in axial length greater than 0.1mm would be fast myopia progressors (i.e., approximately ≥ –0.50D).
Greater Treatment Results with a Higher Add In the Bifocal Lenses in Nearsighted Kids (BLINK) study, treatment with a soft multifocal add power of +2.50D significantly reduced the rate of myopia progression over three years compared to an add power of +1.50D.3
Impact of Lens Treatment Zone in OK In the Variation of Orthokeratology Lens Treatment Zone (VOLTZ) study, a 5mm (versus 6mm) optical zone diameter resulted in a much smaller (3.10mm versus 3.82mm) topographical treatment zone and a significant reduction in axial length progression.4 This result was similar to that of the free paper presented by Jaime Paune titled “Optic Zone in Myopia Control with Ortho-K: Size Matters,” in which a smaller optical zone diameter reduced the topographical plus power ring diameter and slowed axial length elongation better than with standard OK lens designs.
How important is fluorescein pattern evaluation in OK? Based upon the work by Mountford et al5 and the Contact Lens Evidence-based Academic Reports (CLEAR),6 reliably assessing the fluorescein pattern of reverse geometry OK lens designs is challenging, in part because sodium fluorescein does not fluoresce for tear layers less than 20 microns thick. Therefore, fluorescein pattern evaluation is primarily used to exclude the presence of a grossly misfit lens.
Is there a greater effect with atropine combined with OK? According to recent research, axial elongation was slowed by an additional 24% when 0.01% atropine was added to OK for a total reduction of axial length elongation of 76%.7
The Impact of Higher-Order Aberrations and Axial Length Change Higher levels of higher-order aberrations (HOAs), spherical aberration, and positive primary spherical aberration found in young subjects wearing OK lenses were associated with slower axial elongation.8
Finally, in her free paper titled “Patient Reported Outcomes with Orthokeratology Lens Wear,” Erin Tomiyama, OD, determined that long-term patient satisfaction with OK lenses is high for both adults and children. Adults may be more critical in their initial analysis of comfort, vision, and handling, especially if they are established soft contact lens wearers.
• Ortho-K Session
The “Orthokeratology: Reshaping Vision” session featured an educational presentation by Anith Pillai, OD, looking specifically at how OK works. Dr. Pillai emphasized the need for having a topographer to facilitate successful OK outcomes. He shared that the axial map shows the size and effect of the treatment zone, the tangential map is used to visualize shape and make curve modifications, and the refractive map is used to visualize how much correction is achieved.
Also, the elevation map is used during the pre-fit portion when practitioners are in the fitting phase—and when they make the decision to go with a toric or spherical design. Dr. Pillai closed with information on troubleshooting problems, from lateral decentration to central island.
• Myopia Control x Spectacles
In another CE session, titled “Expanding Interventions for Myopic Progression Control – Spectacle-Based Options,” Dr. Dillehay discussed spectacle-based options for myopia control and looked at the key risk factors for myopia. These factors included age, sex, parental myopia, race, amount of time spent indoors/outdoors, and digital device use.
Dr. Dillehay presented numerous studies and papers on the topic, unpacking a focus on solutions that have had limited success with myopia treatment. She then looked at the current spectacle-based solutions, including products such as peripheral plus lens designs.
DECISION-MAKING IN IRREGULAR CORNEA
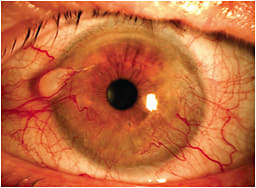
Education about the irregular cornea began on Wednesday evening with the “Corneal Diagnostics and Monitoring for the Contact Lens Practitioner” workshop. During this session, which was co-hosted by the International Keratoconus Academy, S. Barry Eiden, OD; John Gelles, OD; Louise Sclafani, OD; Christine Sindt, OD; and Andrew Morgenstern, OD, reviewed technologies that could be used when evaluating patients’ corneas.
Technologies discussed included Placido topography, ocular surface and dry eye diagnostics, tomography, wavefront aberrometry, specular microscopy, anterior segment photography, corneal genetic testing, and corneal cross-linking. The panelists mentioned that while it isn’t necessarily possible to compare metrics of the same device from different brands, measurements should accurate and repeatable with the same device over time.
However, they emphasized, it is important to remember that even the same brand of device may introduce errors if it is not calibrated routinely. After the lecture portion of the workshop, the attendees broke into five groups and were able to operate the various devices during the wet lab portion of the workshop (Figure 1).

• General Session
An important question in the management of the irregular cornea is when to use the many modalities available to manage these patients. In the general session titled “Irregular Cornea Management in 2022,” speakers Dr. Bennett; Tiffany Andrzejewski, OD; Dr. Gelles; Jennifer Harthan, OD; and Randy Kojima explained the options available and when to use them.
The Role of Corneal Topography Randy Kojima initiated the program with an overview of how corneal topography can help the contact lens specialist decide between scleral and corneal GP lenses. Using the elevation map, he has found that a corneal GP lens can be successfully fit in 88.2% of eyes when the meridian of greatest corneal elevation change is 350 microns or less.9
Corneal Cross-Linking (CXL) It was emphasized that CXL is an invaluable procedure for early progressive keratoconus patients that can greatly slow or halt the progression,10 improve the quality of their lives,11 and offer a significant economic value when it is performed early in the disease process and/or a younger age.12 Patients can typically be fit or return to contact lens wear four weeks after the operation once the epithelium is smooth and illustrious. Corneal haze is sometimes observed after the procedure, and is greatest at one month, plateaus at three months, and significantly decreases between three and 12 months.13
Corneal GP Dr. Bennett indicated that corneal GP lenses—including the larger (10.5mm to 12mm) intralimbal designs—are still an important option today in the fitting of the irregular cornea patient. When the readership of Contact Lens Spectrum was surveyed to determine their preferences in the contact lens management of the irregular cornea, corneal GPs were second (28% as compared to 52%) to scleral lenses as the “go-to” lens option with hybrids (5%), custom soft (4%), and piggyback (1%) being much lower.14 He explained that—in addition to cases of lower elevation difference—individuals with a small or nipple cone, as well as those not interested in, or having failed in, scleral lenses are often good candidates for corneal GP lenses.
Scleral Lenses The Scleral Lenses in Current Ophthalmic Practice (SCOPE) study concluded that sclerals were a very popular form of irregular cornea corrective option, with 74% prescribed for irregular cornea and 16% for dry eye.15 Having greater than 350 microns of elevation difference9 and advanced disease are definite indications for scleral lenses. The impact of sclerals on reducing the need for corneal transplants is very important as well.16
Hybrid Applications Hybrid lenses represent a viable alternative in cases of forme fruste, mild, and moderate keratoconus. Patients who cannot tolerate a corneal GP design, desire more improvement in vision than can be achieved with a custom soft design, or do not desire sclerals are candidates as well.
Custom Soft Custom soft lenses—by virtue of being manufactured in virtually any lens parameter, power, and axis and available in SiHy material—are a viable alternative for many irregular cornea cases, especially in milder forms. Patients should be told that they may have to accept slightly decreased vision in exchange for increased comfort. It is recommended to use relatively flat base curve radii, and to expect up to 1mm to 2mm of movement with the blink.
• Kerataconus Session
Abigail Menner, OD, and Stephanie Pisano, OD, provided a look into the life of a keratoconus patient in their course titled “Beyond the Lens: The Social, Quality of Life, and Financial Implications of Keratoconus.” It is evident that as the disease progresses, the keratoconus patients’ attitude and quality of life are decreased, and the economic burden can add to their stress. They tend to be more pain avoiding, asocial, and anxious.17
Communicating with patients is paramount. Their bottom-line suggestions were to be interested, empathetic, attentive, and supportive; be non-dominant/not intimidating; provide supportive information; do not rush and leave time for questions; convey hope; explain how you and the patient are a team; lay out a plan and direction for the future; and regularly check on the information needs of long-standing patients.
MULTIFOCAL LENSES
An important area of interest pertains to decentered optics on scleral multifocal lenses. In the free paper titled “Visual Quality of Decentered-Optic Multifocal Scleral Lens Design,” Juan Gonzalo Carracedo Rodriguez provided the results of a study comparing a single-vision optics scleral lens, a scleral multifocal lens without decentered optics, and a scleral multifocal lens with decentered optics.
As scleral lenses typically decenter slightly inferior (due to mass) and temporal (due to elevated nasal sclera), the amount of decentration was calculated from the pupillary center. The results indicated that distance vision was slightly better with the decentered optics design, but intermediate, near, and subjective vision were all significantly better with this design than the other two.
• Multifocal Lens Fitting
In their course titled “GP, Hybrid, and Scleral Multifocal Lens Fitting and Problem-Solving,” Dr. Bennett and Tom Quinn, OD, MS, provided applications as well as fitting and problem-solving pearls for each of these modalities. It was noted that multifocal contact lenses (versus over-spectacles and monovision) have become the contact lens modality of choice for 80% of practitioners.18
The benefits of GP multifocals include good-to-great vision, ocular health, astigmatic correction, and applications in dry eye management (i.e., sclerals). Aspheric designs can be fit empirically and can now achieve high add correction. Translating designs, although benefitting from diagnostic fitting, have the benefit of excellent vision at distance and near due to uninterrupted vision.
With aspheric optics now commonly on the front surface, this allows for a reverse geometry design to correct the oblate cornea often associated with post-refractive surgery. Scleral multifocals often have center-near designs but are indicated for the scleral lens wearer who is now presbyopic—no fitting is necessary; just provide the lens parameters, add power, and pupil size to the laboratory—and dry eye patients.
Several recent hybrid improvements now allow for empirical fitting, a center-distance design for the emerging presbyope, a customized more optimally fitted design, and, most recently, an extended depth of focus (EDOF) lens design that presents a wider depth of focus and field, and vision independent of lens decentration.
• Contact Lens Technology
Nick Gidosh, OD, and Stephanie Ramdass, OD, MS, MBA, also emphasized how important multifocal lenses are in contact lens practice today with their course titled “Contact Lens Technology for the New Generation of Presbyopes.” They emphasized how important it is to “Make the Ask” and see whether patients are interested in contact lenses. The answer may be surprising. How to approach the presbyope is important as well as using terms such as “My goal is to decrease your dependency on reading glasses,” and “We are trying to help you have functional vision.”
They emphasized that there are more soft toric multifocal options than ever before. Likewise, GP multifocals represent a huge practice building opportunity. Scleral multifocals are a viable option today, especially as more designs with decentered optics become available.
In the Multifocal Off-center Optics Visual Effectiveness Study (MOOVES) second year update study, it was determined that an average decentration of the optics by 1.75mm resulted in an average of an 8.7 score for distance acuity, 9.0 for near acuity, 8.7 for comfort, and 9.0 for overall experience on a 10-point scale.19
SCLERAL LENSES
Scleral lenses education began with a two-hour scleral lens workshop cohosted by the Scleral Lens Education Society. Elise Kramer, OD; Robert Ensley, OD; Dan Fuller, OD; and Sheila Morrison, OD, MS, presented a short lecture reviewing the principles of advanced scleral lens fitting. The session also included video demonstrations of advanced design principles, imaging the sclera with scleral topographers, and assessing the lenses under the slit lamp.
• Scleral Integration
In “Don’t Leave Me in Isolation! Scleral Lens Integration in Ocular Surface Disease Management,” Gloria Chiu, OD, noted that the main indications for scleral lenses are irregular corneas and ocular surface disease. However, she wondered at what point practitioners should consider sclerals for dry eye? And how should scleral lens use be integrated into therapy? The Tear Film & Ocular Surface Society (TFOS) Dry Eye Workshop II (DEWS II) offers a guideline to this end.20
Dr. Chiu explained that it is important to know the underlying cause of ocular surface disease (OSD) and to understand the role of each treatment modality. Specifically, treatments need to be performed in a specific order and not done in isolation.
The session finished with a series of case studies, some of which recommended scleral lenses with treatment and others that did not. Dr. Chiu pointed out that scleral lenses are not always a first-line therapy for OSD. Rather, OSD patients often require other concurrent therapies that will change over time and will require some trial and error, because OSD can be unpredictable. Most importantly, Dr. Chiu stressed the importance of embracing comanagement of these patients with other specialists when warranted.
• Scleral Lens Fits
In another CE session, “A Deep Dive into Corneal and Scleral Shape Relationships and the Impact on Scleral Lens Fits,” Jason Jedlicka, OD, noted that topography shows the landscape of the cornea; it can tell practitioners the rate of change of curve across the cornea, the high and low points, and whether the eye is optically regular or irregular.
He further explained that in the anterior eye the cornea and sclera are relatively continuous, but that the conjunctiva overlying the sclera is somewhat unpredictable. The sclera gives shape to the eye, but ultimately, the conjunctiva has an influence.
Dr. Jedlicka discussed various imaging technologies and their pluses and minuses. For instance, reflection-based topography interprets the corneal and scleral shape based on the reflection of rings off the front of the eye. However, it is tear dependent, which means the data isn’t always accurate.
With Scheimpflug topography, a slit beam and Scheimpflug camera takes several cross-sectional images of the anterior segment of the eye; it measures elevation and extrapolates curvature. Additionally, it is not tear-layer dependent.
Corneal topography maps the curvature of the eye. But, while it tells how fast things are changing, it doesn’t provide the high and low points. Elevation maps show areas of elevation and depression relative to a “reference sphere” that is generated by the average height of the cornea. Dr. Jedlicka reminded attendees to make sure that reference spheres match when comparing over time and not to forget to match scale, type of map, and reference sphere values from map to map.
Dr. Jedlicka noted that the cornea contributes a significant percentage of the elevation difference in the anterior segment of the eye. Because most scleral lenses compensate for this elevation difference in the scleral landing zone, this can often create suboptimal fitting outcomes.21
Additionally, the shape of the cornea is more oval than spherical, which means that landing precisely the same distance from the limbus is not possible without oval zones. This situation may need quandrant-specific lenses to accommodate the differences in meridional elevations at the inner versus outer landing points.
Corneal shape can also be problematic. Dr. Jedlicka explained that the cornea is usually steeper and thus deeper in one meridian. Therefore, standard scleral lenses will almost always overvault the limbus in one meridian, and lenses will always slide down the steep meridian.
While often a cornea is deeper vertically and shallower horizontally, there is a degree of reversal of that in the sclera in many patients.22 Irregular corneas have more irregular scleras as well.
Dr. Jedlicka concluded that ECPs should consider the shape of the cornea under the scleral lens, utilize elevation maps to know what to expect, and recognize that the limbus is an area of shape change in many patients. He pointed out that scleral lenses really are two lenses in one, the vaulting chamber and the landing zone. To get the best fit, we should try to make the vaulting chamber “end” as uniformly to the sclera as possible.
Think about the corneal zone as an area of fit separate from the scleral zone. Evaluate in primary gaze, no looking up, down, or to the sides (especially when you take an OCT). Finally, push the lens into the position you want it to sit, then evaluate the fitting relationship of lens to eye.
• The Super Session
The final scleral education came on Saturday afternoon during the “Scleral Lens Super Session.” Dr. van der Worp started the session off virtually from the Netherlands with a presentation that looked at the most recent scleral lens research, especially as the number of published reports has increased over the last decade.
He noted that because ECPs have a better understanding about ocular shape, sclerals have become more popular now. One recent report that he highlighted was the recent CLEAR on sclerals.23
Specifically, he pointed to information about settling that occurs after scleral lenses are applied. He also highlighted recent research that discussed compression and rebounding post-scleral lens wear, as well as the composition of midday fogging.
Next, Damien Fisher, PhD, gave his presentation from Australia. He touched on the influence of scleral lenses on corneal edema under open- and closed-eye conditions. Dr. Fisher noted that there are limitations to previous research.
Theoretical model limits exist because the behavior of oxygen and carbon dioxide is difficult to predict; they assume no tear exchange; they typically use central lens thickness only; and they do not necessarily agree with empirical data or clinical experience. In empirical studies, only a narrow range of fluid reservoir thickness has been studied, there is minimal data on closed-eye conditions, there is often a small sample size for lens thickness studies, and there is no study that has measured corneal edema with a lens fenestration.
After examining various studies that looked at those limited areas, Dr. Fisher advised that sclerals should be limited to daily wear unless constant corneal protection is necessary. Practitioners should consider the thinnest practical central fluid reservoir and lens thickness to reduce edema. Additionally, incorporating a lens fenestration could achieve a further reduction.
Next, Dr. Jedlicka noted that properly fit scleral lenses should vault the cornea, should not compress the limbus, and should align with the sclera; the latter is the most complex aspect of the fitting process, he said. He explained that aligning the sclera involves understanding the shape of the eye inside the vaulting chamber and understanding the shape of the eye in the scleral landing zone.21
For the most accurate scleral shape data, discontinue all contact lens wear (including soft lenses or corneal GPs) for at least 36 hours prior. For eyes with any signs of conjunctival abnormality (inflammation, 3-to-9 o’clock staining, edema, chemosis, etc.) treat with a topical steroid for at least a few days prior to imaging as well.
To get scleral shape without shape data, look for edge lift or compression, ask patients about lens awareness, look for lens movement with blink, and manually center a decentered lens to check for alignment issues (especially the aforementioned edge lift). However, if ECPs have ocular surface shape data, they should use it to empirically fit the scleral lens.
Next, Gloria Chiu, OD, noted that to function properly, scleral lenses need cleaners, solutions, and sometimes tools to help apply and remove them from the ocular surface. Scleral lenses should never be filled with preserved saline, preserved artificial tears, GP lens soaking solutions, soft contact lens multipurpose solutions (MPS), GP lens MPS, or peroxide solutions. She concluded her talk with a look at two studies in which she examined the bacteriostatic effect of multidose preservative-free buffered saline and bacterial growth in open saline bottles.24,25 CLS
CONTACT LENS SPECIALTY LENS PRACTICE
GSLS highlighted specialty lens practice in the 2022 program. In the general session moderated by Dr. DeLoss titled, “Specialty Lens Practice in Motion,” three experts shared their knowledge. Stephanie Woo, OD, emphasized staff education that includes how to explain the new services that your office is offering; giving your staff trigger words (e.g., keratoconus, LASIK, etc.); developing scripts they can use when answering patient questions; and helping your staff understand why this new service is important and how it will benefit both patients and the practice.
For scheduling specialty lens patients, it is important to block off 1.5 to two hours for the initial fitting and one to two hours for dispense and application/removal training. Schedule new fits to allow for extra time if necessary (e.g., right before lunch or as the last patient of the day). To build a specialty lens practice, interact with local physicians (i.e., optometrists, ophthalmologists, and other medical specialties) about the need for your specialty.
Jeffrey Sonsino, OD, discussed audits for medically necessary lenses. He emphasized that you need to complete every chart and take the time to do it correctly every time. In addition, it’s not what you bill and code, it’s what you collect after an audit. It is important to minimize what you must pay back to be successful. His “Do’s and Don’ts for Surviving an Audit” are given in Table 2. David Kading, OD, emphasized the importance of the practice website. It will drive people into your practice and should be updated regularly. Have someone qualified to perform search engine optimization (SEO) to ensure your website is accessible by as many people as possible.
Do’s
|
Don’ts
|
• Specialty Lens Practice
In the “Building a Specialty Lens Practice – Taking It to the Next Level” CE breakout session, Drs. Woo, and Kramer expanded upon the ideas from the general session and had a conversation about how they started their specialty lens practices and how they have made them successful. While discussing how to get referrals, Dr. Woo suggested talking to your existing patients.
Both practitioners also mentioned that they both went door-to-door and spoke to other medical professionals when they started out and still do so today; it is often necessary to co-manage patients with other specialists so having that established relationship can be helpful. They also both host what they called “An Evening of Excellence,” which is a cocktail reception for those referring physicians.
Once you get those patients, it’s important to continually market your practice. Dr. Kramer said marketing can come in many forms including newsletters, websites, email blasts. Additionally, she stressed the importance of SEO. “If someone types in ‘Myopia Management’ and you are on page 5 of the search results, you won’t be found,” she said. Dr. Woo noted that having a robust social media presence is also crucial. In addition, Dr. Kramer suggested getting your practice listed on an related organization sites (e.g., GP Lens Institute, National Keratoconus Foundation, or Scleral Lens Education Society). In the end, they emphasized that it is vital to do what is going to make you happy in practice.
The session ended with a question about how they decided to have a practice that exclusively focused on specialty lenses. Dr. Kramer said that she could have done general optometry but determined that her time was better spent on specialty patients. Similarly, Dr. Woo considered what her ideal day would look like, and specialty lenses played a big part of it so that dictated her decision.
POSTER AWARD WINNERS
This year’s Poster Session featured 106 posters on a wide variety of topics, including sclerals, prosthetic contact lenses, corneal disease, keratoconus, orthokeratology, and more. The following were chosen as the best in their categories:*



Research
First Place:Comparing 5mm and 6mm Back Optic Zone Diameter (BOZD) in Orthokeratology Lens Design
Liandra Jung, OD; and Maria Liu, OD, PhD, MPH
Second Place:Instrumentation and Processes for Fitting and Manufacturing Wavefront-guided Soft Contact Lenses for the Highly Aberrated Eye
Jason Marsack, OD, MSc; Raymond Applegate; Paul Pulaski; Matt Haugo; Jeff Kohlberg; Janine Bugno; Keith Parker; Frank Chinisci; and Dan Neal
Third Place:Novel Method of Acanthamoeba Movement Quantification to Determine Efficacy of Contact Lens Care Solutions
Allison Campolo, MS, PhD; Rhonda Walters; Brian Patterson; and Monica Crary
Clinical Case Report/Series
(Optometry resident first author)
First Place:Utilization of Custom Impression-Based Device for Optimal Alignment over Glaucoma Drainage Device and Management of Persistent Corneal Epithelial Defect
Hannah Yoon, OD, MS; and Ellen Shorter, OD
Second Place:Corneal Gas Permeable Lens Management: Post-DSEK and PKP Secondary to Fuch’s Endothelial Corneal Dystrophy
Lauren Zabaleta, OD; and Dawn Lam, MSc, OD
Third Place:Visual Potentials of Wavefront Guided Scleral Lenses in Post Lasik Ectasia: A Case Report
Sabari Arcot, OD
Clinical Cast Report/Series
(Non-optometric resident first author)
First Place:Diagnosing Acanthamoeba in Keratoconic Specialty Contact Lens Wearers
Florencia Yeh, OD; and Brianna Ryff, OD
Second Place:Iris Occlusion Prosthetic Contact Lens for Urrets-Zavalia syndrome
Amanda Dieu, OD
Third Place:The Benefit of Washout and Stabilization when Refitting Ortho K
Siyun Ren; Jayeshwar Nigan; Julie Lin; and Sharon Park Keh, OD
PHOTO AWARD WINNERS


Note: Images appear on the cover of this issue.
SAVE THE DATES!

On June 9 to 11, 2022, Contact Lens Spectrum will present GSLS: Virtual, an extension of the in-person GSLS. This digital event offers the opportunity to stay up to date on best practices and new techniques through interactive, educational sessions streamed conveniently from home. This free program acts as a complement to the in-person January meeting and features many diverse faculty and a new and different agenda. Visit www.clspectrum.com/gsls-virtual for more information.
Then, on Jan. 18 to 23, 2023, the in-person GSLS will be back at Bally’s in Las Vegas. Join us for the same great education presented by industry experts that you’ve come to expect from this event.
REFERENCES
- Yam JC, Li FF, Zhang X, Thamm CC, et al. Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study. Ophthalmology. 2020 Jul;127:910-919.
- Rose LVT, Schulz AM, Graham SL. Use baseline axial length measurements in myopic patients to predict the control of myopia with and without atropine 0.01. PLoS One. 2021 Jul 15;16:e0254061.
- Walline JJ, Walker MK, Mutti DO, Jones-Jordan LA, et al. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children: The BLINK Randomized Clinical Trial. JAMA. 2020 Aug;324:571-580.
- Guo B, Cheung SW, Kojima R, Cho P. One-year results of the variation of orthokeratology lens treatment zone (VOLTZ) study: a prospective randomized clinical trial. Ophthalmic Physiol Opt. 2021 Jul;41:702-714.
- Mountford J, Cho P, Chui WS. Is fluorescein pattern analysis a valid method of assessing the accuracy of reverse geometry lenses for orthokeratology. Clin Exp Optom. 2005 Jan;88:1:33-38.
- Vincent SJ, Cho P, Chan KY, Fadel D, et al. CLEAR – Orthokeratology. Cont Lens Anterior Eye. 2021 Apr;44(2):240-269.
- Wan L, Wei CC, Chen CS, Chang CY, et al. The synergistic effects of orthokeratology and atropine in slowing the progression of myopia. J Clin Med. 2018 Sep 7;7:259.
- Lau JK, Vincent SJ, Cheung SW, Cho P. Higher-order aberrations and axial elongation in myopia children treated with orthokeratology. Invest Ophthalmol Vis Sci. 2020 Feb;61:22.
- Zheng F, Caroline P, Kojima R, Kinoshita B, Andre M, Lampa M. Corneal elevation differences and the initial selection of corneal and scleral contact lens. Poster presented at the 2015 Global Specialty Lens Symposium, January 2015, Las Vegas.
- Hersh PS, Stulting RD, Muller D, Durrie DS, Rajpal RK; United States Crosslinking Study Group. United States Multicenter Clinical Trial of Corneal Collagen Crosslinking for Keratoconus Treatment. Ophthalmology. 2017 Sep;124:1259-1270.
- Brooks NO, Greenstein S, Fry K, Hersh PS. Patient subjective visual function after corneal collagen crosslinking for keratoconus and corneal ectasia. J Cataract Refract Surg. 2012 Apr; 38:615-619.
- Lindstrom RL, Berdahl JP, Donnenfeld ED, Thompson V, et al. Corneal crosslinking versus conventional management for keratoconus: a lifetime economic model. J Med Econ. 2021Jan-Dec;24:410-420.
- Greenstein SA, Fry KL, Bhatt J, Hersh PS. Natural history of corneal haze after collagen crosslinking for keratoconus and corneal ectasia: Scheimpflug and biomicroscopic analysis. J Cataract Refract Surg. 2010 Dec;36:2105-2014.
- Bennett ES. GP Annual Report. Contact Lens Spectrum. 2020 Oct;35:28-30,32,34,36,37,59.
- Nau CB, Harthan J, Shorter E, Barr J, et al. Demographic characteristic and prescribing patterns of scleral lens fitters: The SCOPE study. Eye Contact Lens. 2018 Sep;44 Suppl:S265-S272.
- Koppen C, Kreps EO, Anthinissen L, Van Hoey M, Dhubhghaill SN, Vermeulen L. Scleral Lenses Reduce the Need for Corneal Transplants in Severe Keratoconus. Am J Ophthalmol. 2018 Jan;185:43-47.
- Moreira LB, Alchieri JC, Belfort R, Moreira H. [Psychological and social aspects of patients with keratoconus]. [Article in Portugese] Arq. Bras. Oftalmol. 2007 Mar-Apr;70:317-322.
- Nichols J, Starcher L. Contact Lenses 2021. Contact Lens Spectrum. 2022 Jan;37:22-24,26,28,29.
- Gidosh N. Multifocal Off-center Optics Visual Effectiveness Study (MOOVES): 2nd year update. Presented at: Virtual Global Specialty Lens Symposium, January 2021, Las Vegas.
- Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017 Oct;15:802-812.)
- Jedlicka J, Gee S. Meridional Differences in Sagittal Height at 12 mm and 16 mm chords. Poster presented at the 2020 Global Specialty Lens Symposium, January 2020, Las Vegas. Available at https://bit.ly/37iMiok . Accessed Mar. 1, 2022.
- Siebert S, Jedlicka J. Utilizing corneal topography to aid in predicting scleral topography for the purpose of fitting scleral contact lenses. Poster presented at the 2017 Global Specialty Lens Symposium, January 2017, Las Vegas.
- Barnett M, Courey C, Fadel D, et al. BCLA CLEAR – Scleral lenses. Cont Lens Anterior Eye. 2022 Apr;44:270-288.
- Seo W, Chiu GB, She RC. Bacteriostatic Effect of Multipurpose Preservative-free Buffered Saline Use in Scleral Lens Wear. Optom Vis Sci. 2020 Mar;97:162-168.
- Jeong M, Lee KL, She RC, Chiu GB. Microbial Evaluation of Opened Saline bottles for scleral lens use and hygiene habits of scleral lens patients. Optom Vis Sci. 2021 Mar 1;98:250-257.




