A post-penetrating keratoplasty (PK) patient developed conjunctival prolapse after wearing a scleral lens in OD.
History
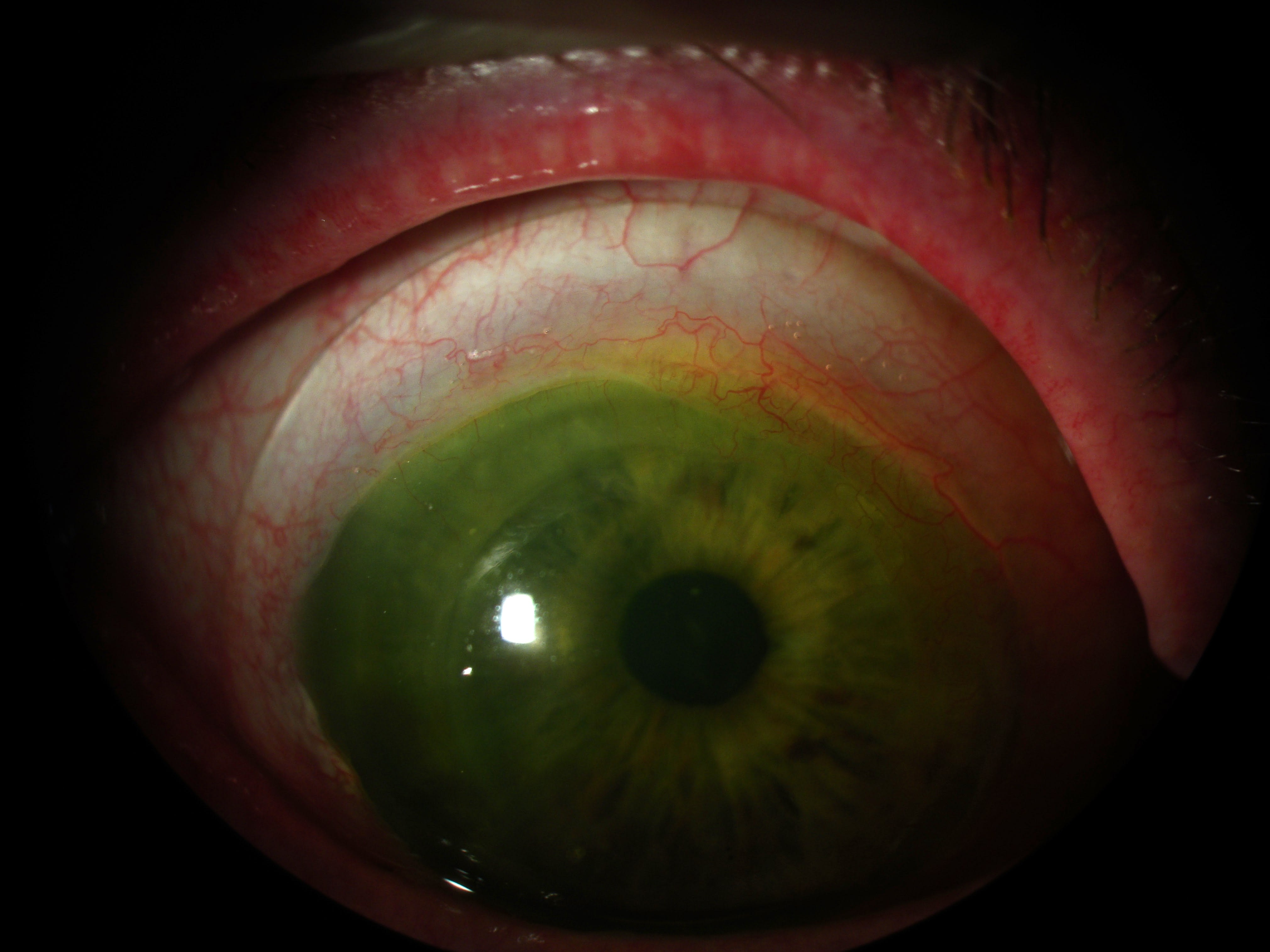
A 74-year-old male underwent PK more than 20 years ago and wore a small corneal GP lens for many years for the resulting corneal irregularity. In 2024, he was fitted with a 16.5 mm specialty scleral lens. At follow-up, OD showed conjunctival prolapse; OS remained stable. A haptic modification to improve scleral alignment was unsuccessful.
Scleral lens parameters were: base curve (BC) 50 D x 46 D (6.75 mm x 7.34 mm), power of –6.50 D, overall diameter (OAD) of 16.5 mm, optic zones of (OZs) 11.5 mm/13.9 mm, SAG of 6,258 μm, and Dk of 200.
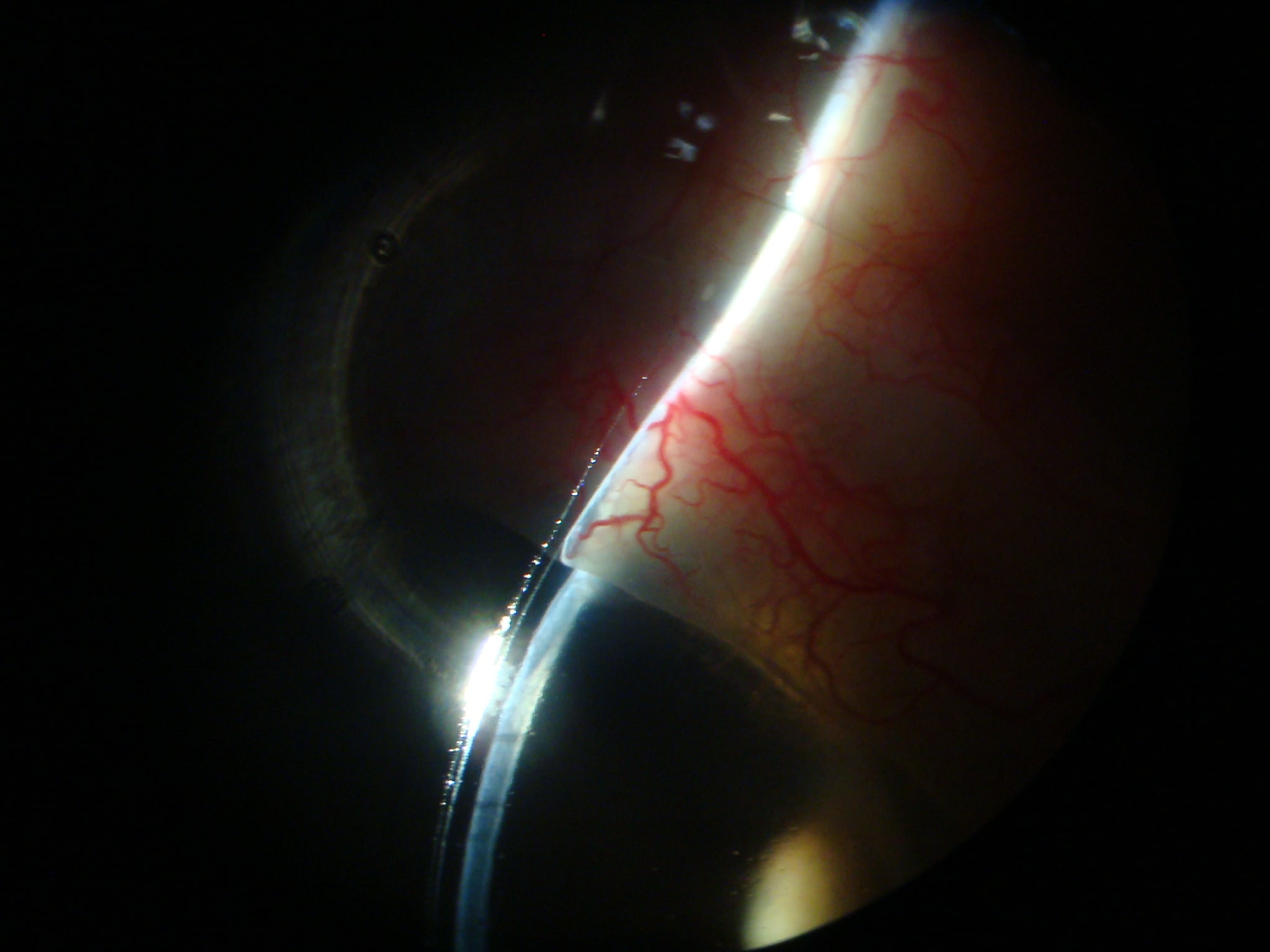
The patient alternated between the corneal GP and scleral lens to minimize symptoms. Slit lamp evaluation showed excessive clearance centrally and over the limbus (Figure 1).

The post-graft elevation required vaulting, with the central cornea flatter than the periphery.
Conjunctival prolapse, more common in the elderly, results from loose conjunctival tissue that prolapses over the cornea when under a scleral lens. It is believed to result from negative pressure forces under a scleral lens, particularly in lenses without a uniform tear reservoir (Walter et al, 2016).
In this patient, prolapse was likely exacerbated by excessive superior vault. The large amount of superior vault was due to high overall vault and a landing zone transition not optimized for the shape of the corneal graft to sclera (Figure 2).
Anterior tomography maps confirmed a flat central area (graft) and steep periphery (Figures 3-5).



Customized Adjustments of the Scleral Lens Design
The redesigned scleral lens redesigned had the following parameters: BC of 49 D x 47 D (6.89 mm x 7.18 mm), power of –6.00 D, OAD of 16.5 mm, OZs of 12.0 mm/13.5 mm,
SAG 6,005 μm, and Dk of 200.
Vault was reduced centrally by 253 μm and increased at the midperiphery. The haptic was shortened and realigned closer to the limbus (Figures 6 to 8). Early improvement in prolapse was noted; further assessment will follow lens settling.


After lens settling, less clearance was expected. Observation right after lens application still showed high overall, but more uniform clearance (Figure 9).

Conclusion
In this patient, conjunctival prolapse was improved by reducing excessive central vault and designing a haptic landing zone that decreases excessive peripheral vault in the area of the prolapse.
Bibliography
Walker M, Caroline P, Kinoshita B, Lampa M, Andre M, Kojima R. A proposed mechanism for scleral lens-induced conjunctival prolapse. Poster presented at: Global Specialty Lens Symposium; 2014; Las Vegas, NV.
Caroline P, Andre M. Conjunctival prolapse, hooding, chalasis or… Contact Lens Spectrum. 2012;27(4):56. clspectrum.com/issues/2012/april/contact-lens-case-reports
Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long-term outcomes. Cont Lens Anterior Eye. 2014;37(3):196-202. doi: 10.1016/j.clae.2013.11.001
Fadel D. Scleral Lens Issues and Complications: Their Recognition, Etiology and Management. Dougmar Publishing Group Inc.; 2020:49-52.
Schornack M. Scleral Lenses. In: Fadel D, Barnett M, eds. Specialty Contact Lenses. 2025:109. Elsevier Inc.
Girard LJ, Soper JW. Flush-fitting scleral contact lenses. Am J Ophthalmol. 1966;61(5 Pt 2):1109-1123. doi: 10.1016/0002-9394(66)90232-7
Ridley F. Contact Lens Fitting – theoretical considerations. In: Girard LJ, Soper JW, Gunn C. Corneal and Scleral Contact Lenses. Proceedings of the International Congress. The C.V. Mosby Company; 1967. Chapter 24:214.



