SPECIALTY SOFT LENSES are often indicated for patients who see well with a spectacle refraction but would require a contact lens power that is out of the range of standard soft lenses. Patients who have aphakia, high regular astigmatism, or pathologic myopia, and those who are critical observers, can benefit from custom specialty soft lenses.
Soft lenses mechanically interact with the cornea and reduce the amount of oxygen that reaches the tissue (Jeng et al, 2011). New soft lens materials like silicone hydrogel allow more oxygen to pass through to the cornea. For all contact lens patients, observation under the slit lamp of the limbal region after lens wear is critical to monitoring the health of the cornea and, more specifically, the limbus.
The limbus is known as the gatekeeper that prevents the conjunctival epithelial cells from invading the cornea (Jeng et al, 2011). Limbal stem cells provide the source cells that eventually change to replace the corneal epithelium, which is shed via normal cell turnover (Rossen et al, 2016).
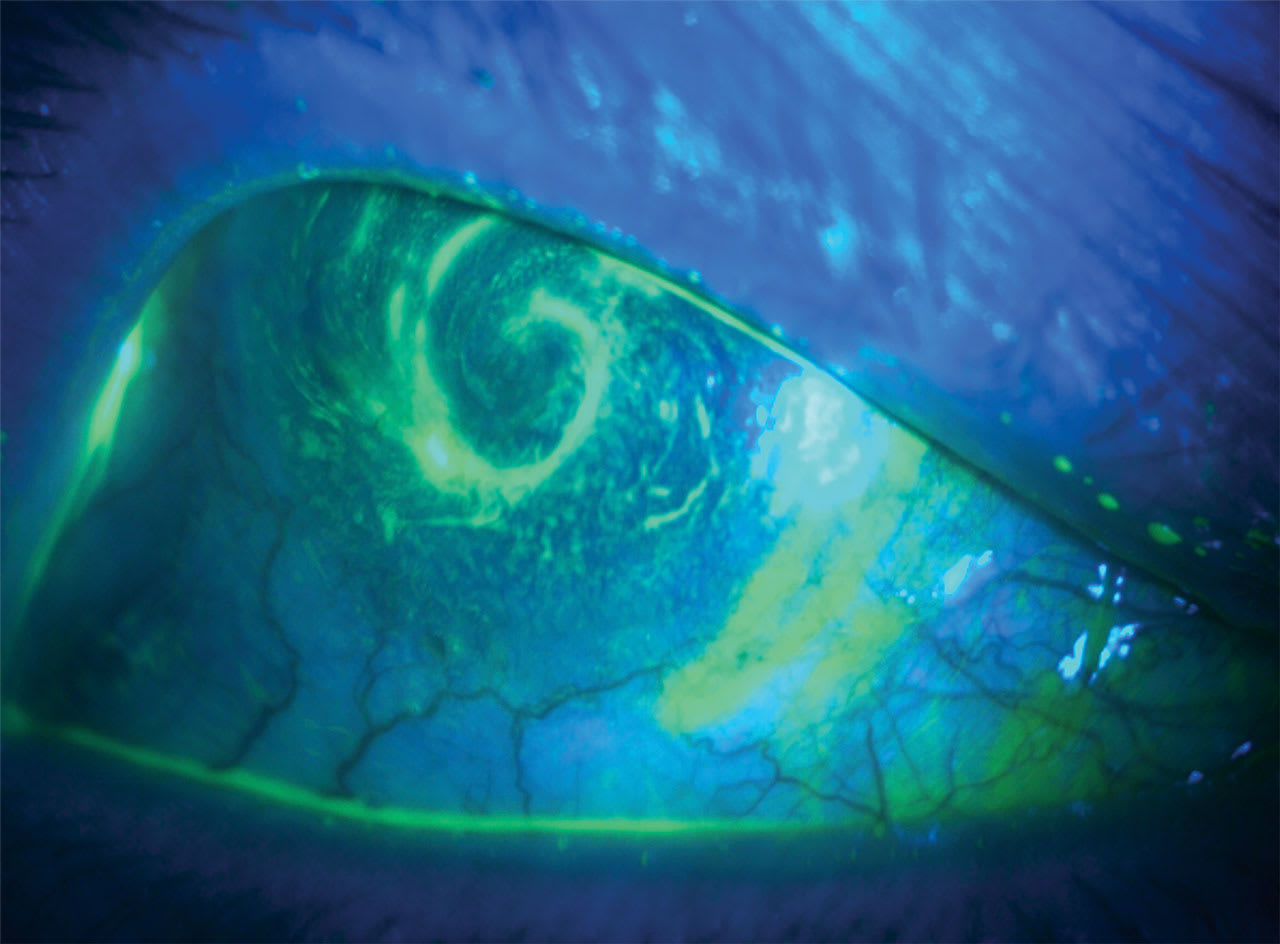
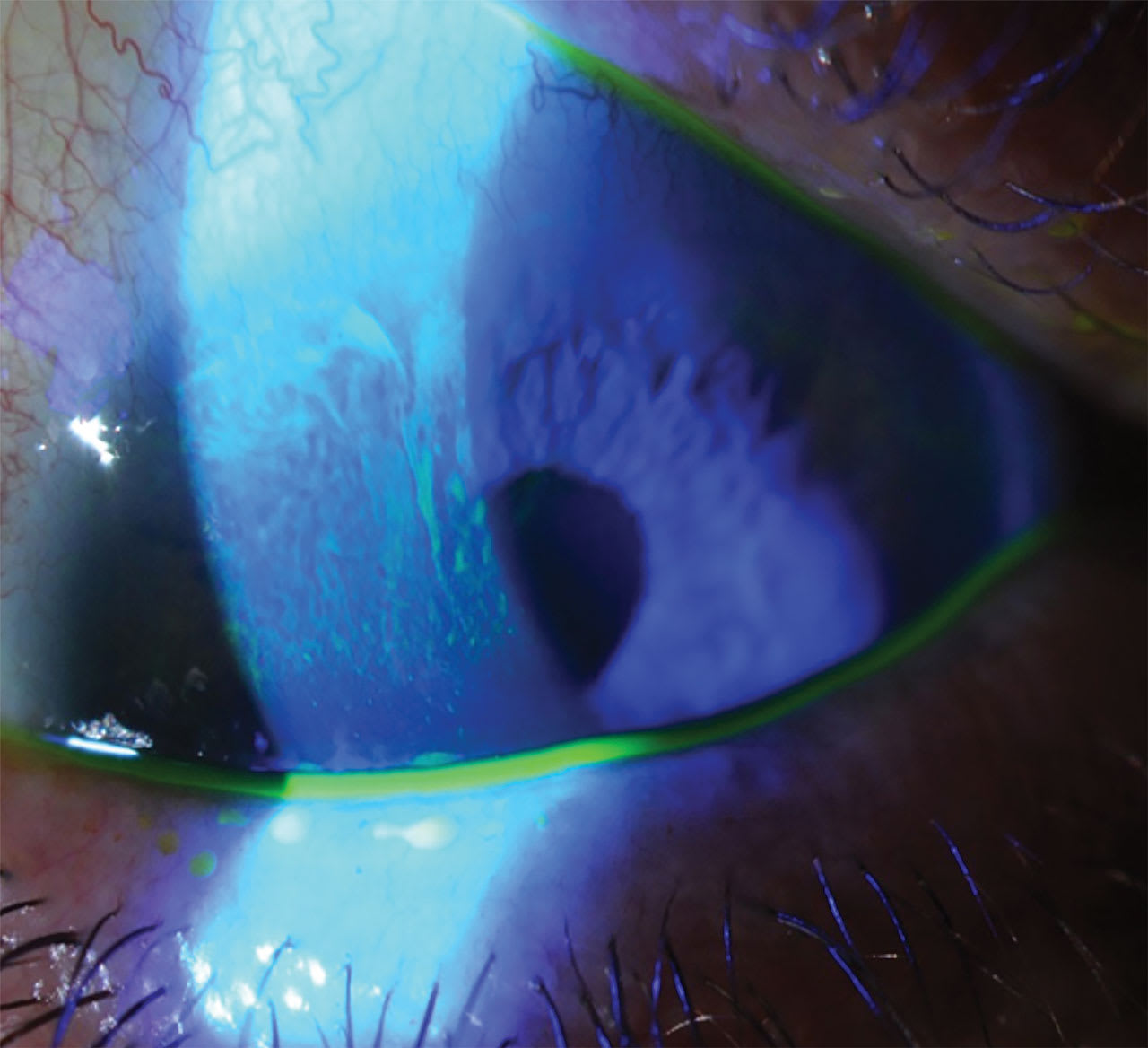
If this process is disrupted and eventually becomes nonfunctional, limbal stem cell deficiency (LSCD) results (Rossen et al, 2016). LSCD has multiple etiologies, and one study found that 16.8% of LSCD cases were secondary to contact lens wear (Cheung et al, 2021). LSCD can be identified clinically with varying presentations including corneal neovascularization, persistent epithelial defects, and several degrees of whorl or late fluorescein staining (Jeng et al, 2011; Cheung et al, 2021) (Figures 1 and 2). Limbal late or whorl staining is due to uptake of the conjunctival epithelium cells that have crossed over to the cornea and hold fluorescein dye longer than healthy corneal epithelial cells (Kim and Mian, 2017).
Because many LSCD patients are asymptomatic in early stages (Jeng et al, 2011), it is critical to remove contact lenses at every office visit and perform a fluorescein stain test to observe late staining or abnormalities of the limbus. Many early cases are treated with cessation of lens wear and topical therapies, while more advanced cases require amniotic membranes, limbal transplants, and scleral lenses (Jeng et al, 2011; Rossen et al, 2016).
In soft contact lens patients, LSCD is commonly seen superiorly first due to repeated mechanical interaction of the lens and the limbus and decreased oxygen to the limbal region (Jeng et al, 2011).
Holden and Mertz (1984) discussed the need for adequate oxygenation during lens wear, based upon the ratio of the lens material oxygen permeability/thickness (Dk/t). They found that the open eye requires lenses with a Dk/t of 24, and a closed eye requires a Dk/t of 87 to avoid corneal edema. Later publications suggest improved methods to measure oxygen dynamics in the cornea and postulate updating the open-eye Dk/t value of contact lenses to 125 to avoid edema (Papas, 1998; Fonn and Bruce, 2005).
The lens Dk/t is directly impacted by the power. Higher myopic lenses are thicker in the periphery, reducing the oxygen to the limbus, and higher hyperopic lenses are thicker in the central area (Yeung et al, 2018).
Most specialty soft lens patients wear custom designs due to high prescriptions and, thus, are at higher risk for LSCD due to lower Dk/t values. Key management strategies that practitioners can implement to lower the risk of LSCD include the use of silicone hydrogel materials, preservative-free disinfection, and slit lamp exams at least once a year to monitor corneal staining so early intervention is possible if signs of LSCD are observed.
References
1. Jeng BH, Halfpenny CP, Meisler DM, Stock EL. Management of focal limbal stem cell deficiency associated with soft contact lens wear. Cornea. 2011 Jan;30(1):18-23. doi: 10.1097/ICO.0b013e3181e2d0f5
2. Rossen J, Amram A, Milani B, et al. Contact lens-induced limbal stem cell deficiency. Ocul Surf. 2016 Oct;14(4):419-434. doi: 10.1016/j.jtos.2016.06.003
3. Cheung AY, Sarnicola E, Denny MR, Sepsakos L, Auteri NJ, Holland EJ. Limbal stem cell deficiency: demographics and clinical characteristics of a large retrospective series at a single tertiary referral center. Cornea. 2021 Dec 1;40(12):1525-1531. doi: 10.1097/ICO.0000000000002770
4. Kim KH, Mian SI. Diagnosis of corneal limbal stem cell deficiency. Curr Opin Ophthalmol. 2017 Jul;28(4):355-362. doi: 10.1097/ICU.0000000000000387
5. Holden BA, Mertz G. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984;25:1161-1167
6. Papas E. On the relationship between soft contact lens oxygen transmissibility and induced limbal hyperaemia. Exp Eye Res. 1998;67:125-131. doi: 10.1006/exer.1998.0504
7. Fonn D, Bruce AS. A review of the Holden-Mertz criteria for critical oxygen transmission. Eye Contact Lens. 2005 Nov;31(6):247-51. doi: 10.1097/01.icl.0000182488.70745.1d
8. Yeung KK, Yang HJ, Nguyen AL, Weissman BA. Critical Contact Lens Oxygen Transmissibility and Tear Lens Oxygen Tension to Preclude Corneal Neovascularization. Eye Contact Lens. 2018 Sep;44 Suppl 1:S291-S295. doi: 10.1097/ICL.0000000000000412



