Myopia has become increasingly more prevalent as an ocular disorder. There have been several clinical strategies developed to slow myopia progression, one of which is orthokeratology (ortho-k). Orthokeratology is a reverse geometry corneal GP lens that flattens the central cornea and steepens the mid-peripheral cornea. The aspheric alteration to the cornea induces a hyperopic central refractive shift and a relative myopic shift in the peripheral refraction, inducing peripheral myopic defocus that is believed to inhibit axial length elongation. Ortho-k is at the forefront of myopia management due to its treatment efficacy at slowing axial length, ranging from 36% to 46%.1-3
The ability to evaluate and describe a lens fit remains imperative for troubleshooting. Traditionally, ortho-k lenses were fit primarily with diagnostic fitting sets or with a manufacturer’s nomogram based on flat keratometry values and manifest refraction. While this approach provided positive results, it could be very time consuming and is reliant on a provider's clinical experience.
This article will discuss how 2 other methods of evaluating ortho-k lens fits—slit lamp/anterior segment imaging and topography—can be used to achieve effective and more efficient fitting and follow-up processes.
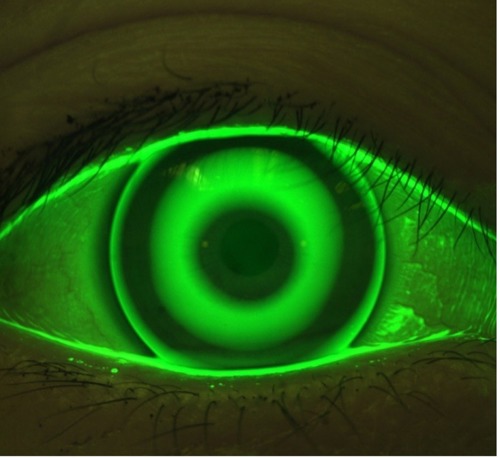
Slit Lamp/Anterior Segment Evaluation
One option to evaluate the fitting characteristics of ortho-k lenses is via the slit lamp or anterior segment imagining. By utilizing dynamic fluorescein evaluation, an ideal fitting ortho-k lens displays a characteristic bull’s-eye pattern. This represents a central base curve or treatment curve, a surrounding return zone that is key for centration, and a peripheral landing zone that is used to provide the appropriate edge alignment and tear exchange.
Slit lamp imaging can be a useful tool to monitor lens fit over several visits, but it can also be an invaluable tool to send to consultation. Consultation can be particularly helpful in determining what parameter needs to be changed with ortho-k to improve centration and patient outcomes (Figure 1).
Advances in corneal topography allow many ortho-k lens designs to be fit empirically by providing manufacturers with valuable information on corneal curvature, diameter, and eccentricity.2 Axial difference maps can be utilized to illustrate changes in refractive power, and tangential difference maps can be used to illustrate the positioning of the ortho-k lens.
Evaluation of difference map displays during the ortho-k fitting process may free patients from wearing their ortho-k lenses to follow-up examinations. Central flattening, paracentral steepening, and lens centration can all be appreciated on a topography tangential map (Figure 2). During nighttime wear, ortho-k lenses position toward the steepest part of the cornea. Low-to-moderate decentration of the ortho-k lens is common due to the temporal corneal shape being steeper than the nasal cornea.3
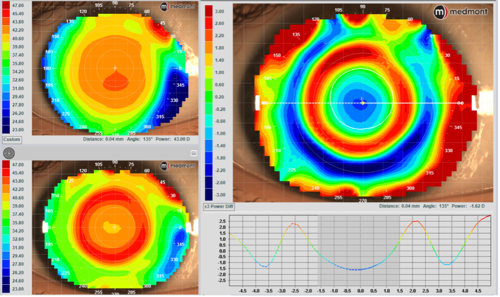
Topography advances also allow for ortho-k lens customizations that can be useful throughout the fitting process. By evaluating elevation differences between the flat and steep meridians at an 8 mm chord, it can be determined if a toric ortho-k lens would be beneficial.4 A sagittal height difference of 25 µm to 30 µm or more indicates a toric lens should be ordered.
Additionally, a smaller treatment (ie, back-surface optical) zone diameter has been shown to improve myopia management efficacy, further reducing axial length elongation. The back optical zone diameter considers pupil diameter. While the standard back optic zone diameter in most lens designs is 6.0 mm to 6.2 mm, a back optic zone diameter of 5.0 mm has been shown to be 31.38% more effective in slowing axial length over a 12-month period.2
Diagnostic imaging can play a vital role in fitting and evaluating ortho-k lenses. To achieve optimal vision and slowing of axial length, slit lamp/anterior segment imaging and topography can all be utilized during the fitting and follow-up processes.
References
- Chen Z, Zhang Z, Xue F, et al. The relationship between myopia progression and axial elongation in children wearing orthokeratology contact lenses. Cont Lens Anterior Eye. 2023;46(1):101517. doi:10.1016/j.clae.2021.101517
- Wu J, Zhang X, Wang L, Zhang P, Guo X, Xie P. Altering optical zone diameter, reverse curve width, and compression factor: impacts on visual performance and axial elongation in orthokeratology. Cont Lens Anterior Eye. 2024;47(3):102136. doi:10.1016/j.clae.2024.102136
- Liu T, Ma W, Wang J, et al. The effects of base curve aspheric orthokeratology lenses on corneal topography and peripheral refraction: A randomized prospective trial. Cont Lens Anterior Eye. 2023;46(3):101814. doi:10.1016/j.clae.2023.101814
- Fan Y, Yu Z, Tang T, et al. Machine learning algorithm improves accuracy of ortho-K lens fitting in vision shaping treatment. Cont Lens Anterior Eye. 2022;45(3):101474. doi:10.1016/j.clae.2021.101474
This content was supported via unrestricted sponsorship




