Orthokeratology (ortho-k) has become the preferred method for managing myopic refractive error in my pediatric patients. The refractive and ocular benefits of ortho-k are well established; however, it has been labeled a complicated and time-consuming niche service. Herein, a case study is presented that describes refractive correction of a young patient’s myopia with Arise orthokeratology lenses (Bausch + Lomb) and demonstrates how efficiently ortho-k can fit into many styles of optometric practice.
Case Description
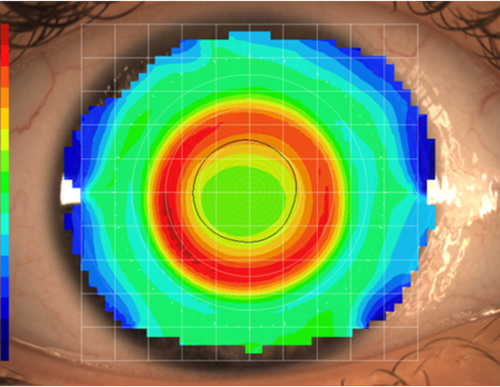
NB, a 12-year-old female patient, presented to our clinic after experiencing changes in her refractive error. Her mother has a history of high myopia, and ortho-k was recommended by the referring provider. NB’s refractive error was -5.00 DS in both eyes. After high-quality topography images were obtained, a cloud-based software was utilized to design lenses with customized optical zones, peripheral curves, and overall diameters.
The platform identified that despite minimal astigmatism in the patient’s refractive error, there were elevation differences between the vertical and horizontal meridians of the cornea, which warranted the use of toric peripheral curves to best center the lens. Due to her age and refractive error, the system also decreased the back optic zone diameter (BOZD). Smaller BOZDs are often used in those with higher myopia for optimal refractive error management. Finally, the lenses were designed to have a custom overall diameter based on the patient’s corneal size.
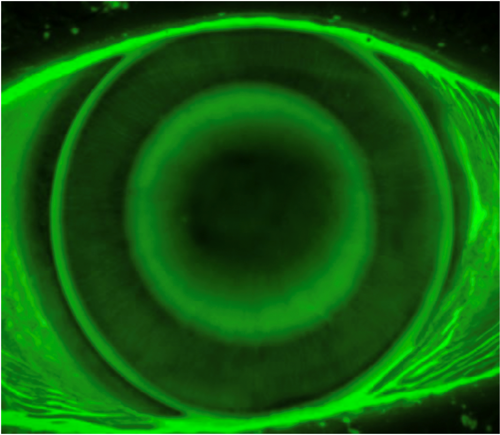
At the dispense visit, the lenses were placed on each eye. Visual acuity was 20/20 through each lens, and over-refraction yielded 20/20 with +0.75 OD and OS. Fluorescein pattern assessment showed an aligned central treatment zone with a centered bullseye ring and aligned peripheral curves. There was mild edge lift and adequate movement on blink to promote tear exchange. The lens fit was deemed acceptable in both eyes, and lenses were dispensed after the patient received training on lens care and handling.
At the 10-day follow-up visit, visual acuity was 20/15 in each eye with a small hyperopic manifest refraction. Her corneas had no findings related to keratitis and no problematic signs or symptoms related to corneal lens wear, and lens handling was reported as excellent.
Discussion
Ortho-k design platforms utilize corneal parameters beyond the traditional measurements of keratometry readings and refractive errors. When additional corneal information such as elevation differences at the opposing major meridians, corneal eccentricity, and corneal diameter are considered, the sagittal depth and peripheral curve toricity can be designed to better match the corneal surface for a more centered treatment zone.
As you can see, in the time it took to capture a topography map, an ortho-k lens can be designed with customized peripheral curves, optical zone, and overall diameters, along with other parameters. The clinical beauty of this platform is that providers can modify suggested lens parameters when desired yet utilize design algorithms as needed for optimal outcomes.
To hear Dr. Messer discuss this case, click here.