A 55-year-old female patient with a history of bilateral radial keratotomy (RK) performed
25 years previously presented with progressive visual deterioration. She previously declined contact lens use, but she is reconsidering due to significant vision loss.
Case Description
Uncorrected visual acuity was 20/200 OD and 20/400 OS. Elevation-based tomography revealed markedly irregular corneas with abrupt central flattening and asymmetric peripheral elevations. Best-corrected visual acuity (BCVA) was 20/80 OD and 20/60 OS. Slit lamp examination showed radial and arcuate scars, superficial epithelial staining, central stromal edema, moderate conjunctival hyperemia, and meibomian gland dysfunction.
Intraocular pressure (IOP) measured 22 mmHg OD and 24 mmHg OS. Corneal pachymetry revealed increased thickness. Endothelial cell count showed reduced density, decreased hexagonality, and elevated coefficient of variation, which indicated significant endothelial structural compromise. Due to edema, increased pachymetry, and elevated IOP, the patient was referred for joint management with cornea and glaucoma specialists.
A corneal specialist resolved the edema with pharmacologic treatment. Scleral lenses were contraindicated due to low endothelial cell density and morphometric deterioration and minimal tear exchange. Corneal GP lenses with reverse geometry were recommended instead. A glaucoma specialist confirmed bilateral open-angle glaucoma, with structural damage evidenced by optical coherence tomography (OCT) and visual field testing. Topical treatment was initiated. Scleral lenses were contraindicated to maintain IOP control.
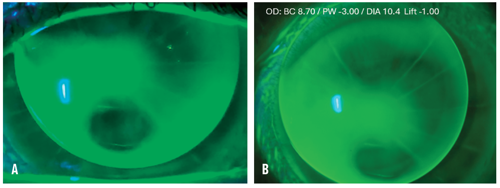
For the corneal lens fitting, the ROSE K2 PG (Menicon) design was selected due to the oblate postsurgical corneas. For the right eye, a diagnostic lens with base curve (BC) of 9.00 mm showed acceptable centration, central pooling, superior and inferior bearing, and peripheral lift. Over-refraction yielded 20/30 VA. The final fit used BC 8.70 mm and reduced edge lift to optimize alignment, resulting in an appropriate fluorescein pattern.
The left eye diagnostic lens was trialed with a BC of 9.00 mm and demonstrated good centration, central pooling, and mild inferior touch. Over-refraction achieved 20/25 VA. The BC was slightly adjusted to reduce the bearing at the highest inferior point, yielding optimal alignment.
Monthly follow-up visits were conducted over 6 months. Final BCVA was 20/30 OD and 20/25 OS. The patient reported excellent comfort (9/10) with 9-10 hours of daily wear. No epithelial staining was observed upon lens removal. IOP remained stable (19 mmHg OD, 18 mmHg OS).
Discussion
In post-RK patients presenting with corneal edema, low endothelial cell density, and glaucoma, lens selection must prioritize ocular physiology and IOP control. In this case, the use of corneal GP lenses with reverse geometry was mandatory to provide proper alignment, high oxygen accessibility, and excellent visual quality without compromising endothelial function or IOP stability. Scleral lenses, while effective in many irregular cornea cases, were contraindicated due to limited tear exchange and potential impact on glaucoma monitoring.
Conclusion
A multidisciplinary approach and close follow-up were essential to achieve a successful, comfortable, and safe contact lens fitting and ensure visual rehabilitation and long-term corneal health preservation.
To hear Dr. Flores discuss this case, click here.