Scleral lenses have continued to gain wide acceptance in managing a multitude of ocular diseases, even in the absence of classic ectatic disorders. Their ability to stabilize vision and provide good comfort makes scleral lenses an increasingly preferred solution when soft or corneal gas permeable (GP) lenses fail. However, landing zone (LZ) interactions from anatomical elevations such as pingueculas, pterygia, scleral patch grafts, and blebs remain a key challenge in fitting. LZ notching should be considered a standard customization tool for optimizing fit and improving patient outcomes.
Case Description
A 63-year-old white male patient was referred for a specialty contact lens fitting due to irregular astigmatism and longstanding failure with soft and GP lenses. He reported fluctuating blurry vision and worsening nighttime glare in both eyes. His best-corrected visual acuity in eyeglasses was 20/30-2 OD and 20/30-1 OS with the following refraction: -4.75 +3.75 x 096 OD and -5.75 +4.75 x 100 OS.
Slit lamp examination revealed clear corneas, mild meibomian gland dysfunction, and mild age-related cataracts. Posterior segment evaluation was unremarkable. Corneal tomography showed no signs of ectasia, with simulated keratometry readings of 41.50/45.25@084 OD and 41.75/46.00@100 OS.
Given the patient’s need for improved visual stability over soft lenses and improved comfort over GP lenses,1 we proceeded with fitting Onefit MED scleral lenses (Blanchard/CooperVision). This design allowed for quadrant-specific haptics, front surface toric optics, and the easy addition of an LZ notch.
The initial fitting process required 3 sets of lenses for each eye to optimize vision and comfort. The final OD lens was designed at 16.0 mm diameter with 125 µm of limbal vault to address limbal microcystic edema seen with the first lens design. Quadrant-specific haptics ensured centration, and a front surface toric correction resolved residual lenticular astigmatism. A similar design was used for the OS lens, yielding 20/20 vision and full-day comfort.
Discussion
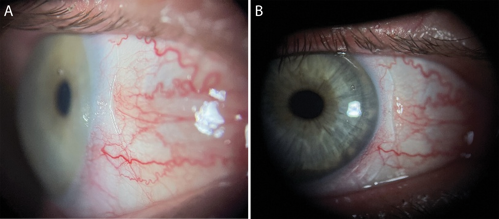
At his 1-year follow-up visit, the patient reported persistent lens awareness and redness OD only after prolonged wear. Slit lamp examination revealed nasal “toe” blanching at the 3 o’clock position consistent with pinguecula impingement (see Figure 1a). To reduce localized mechanical stress and improve lens comfort,2 a 0.5 mm deep x 4.0 mm chord notch was added. Notch depth was measured via anterior segment optical coherence tomography (OCT), and chord length was determined at the slit lamp. This change resolved the patient’s symptoms and maintained 20/20 vision in one lens remake (see Figure 1b).
Conclusion
Scleral lens customization is valuable for patients with nonectatic irregular astigmatism and peripheral landing zone challenges. Notching is a highly effective strategy to accommodate anatomical obstacles without compromising lens fit or stability. As technology evolves and accessibility improves, notching should be embraced as a standard part of scleral lens design in clinical practice.
References
- Nau CB, Schornack M, Harthan JS, et al. SCOPE study: experience of keratoconus patients wearing RGP or scleral lenses. Invest Ophthalmol Vis Sci. 2018;59(9):1778.
- Walker MK, Schornack MM, Vincent SJ. Anatomical and physiological considerations in scleral lens wear: conjunctiva and sclera. Cont Lens Anterior Eye. July 2020. doi:10.1016/j.clae.2020.06.005
To hear Dr. Pickens discuss this case, click here.