Contact lenses remain a mainstay in the visual rehabilitation of patients with keratoconus. However, not all patients achieve success with typical modalities due to issues such as discomfort, poor lens tolerance, or suboptimal visual outcomes. This case report discusses a patient with keratoconus who experienced failure with conventional lens designs and his experience with a custom soft lens specifically designed to address irregular astigmatism.
Case Description
A 43-year-old Hispanic male patient presented to our clinic for evaluation of blurry vision at near distances with habitual corneal gas permeable lenses (GPs), which he had been most recently using only for driving because the lenses caused discomfort. He reported that he was happy with his habitual eyeglasses, which he wore when not wearing the GPs (ie, throughout the rest of the day), and he was interested in other contact lens options. He was previously diagnosed with astigmatism, presbyopia, and vitreous floaters.
The patient’s medical history was positive for seasonal allergies. He denied any ocular surgical history. His social history was unremarkable. He had a family medical history positive for diabetes (mother) and was not taking any systemic medications.
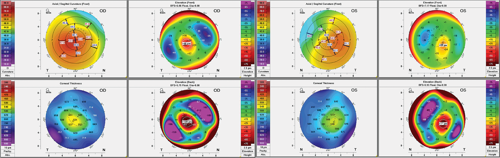
The patient’s keratometry was 58.40/53.62@063 OD and 48.59/45.64@042 OS. The horizontal visible iris diameter (HVID) was 12.0 mm in each eye. Manifest refraction was +0.50 -3.75 x 075 OD and -0.25 -2.75 x 155 OS with a best- corrected visual acuity (BCVA) of 20/125 OD and 20/30 OS with a +1.00DS add for near visual acuity (VA) of 20/25. Entrance pupil testing was within normal limits. Slit lamp biomicroscopy showed a papillary response on the palpebral conjunctiva and apical corneal thinning OD and OS with no scarring. Corneal topography confirmed a diagnosis of severe keratoconus OD and moderate keratoconus OS. Intraocular pressure (IOP) was 14 mmHg in each eye. Dilated fundoscopy was unremarkable.
The patient was diagnosed with keratoconus. Since the patient was already a habitual GP lens wearer and expressed interest in soft contact lens options, we offered a specialty soft lens design. We applied diagnostic specialty soft lenses (KeraSoft Thin, Metro Optics) in parameters 8.6/14.5/PL/STD OD and 8.6/14.5/PL/STD OS. Starting from an autorefraction, we refined to an endpoint overrefraction of -2.75 -2.00 x 080 OD with a VA of 20/20-3 and +1.75 -1.50 x 180 OS with a VA of 20/20. The patient noted vision was clearer after the blink.
There was 1.0 mm of movement in each eye, and the lens was well-centered in each eye. The rotation was stable at 5° left OD, OS. Comfort was excellent, and the lenses were ordered. At dispense, the fit was similar to the diagnostic fit, and lenses were dispensed following application and removal training. Since vision was clearer after the blink, the lens could be too steep. We made a note to monitor whether a flatter lens was necessary at follow-up.
Discussion
At the follow-up visit, vision was stable with no over-refraction. There was no corneal compromise after lens removal. The remaining supply was ordered, and we advised the patient to return in 1 year.
Conclusion
Eight years following the initial fit, the patient is still happy in these specialty soft lenses. The parameters have changed slightly over the years, as his keratoconus has progressed and cataracts have developed. The current lens parameters are 8.4/14.5/STD/-1.00 -1.25 x 168 OD and 8.6/14.5/STD/+1.00DS OS. He is still comfortably wearing these lenses 5 days a week for about 6 hours a day.
To hear Dr. Sicks discuss this case, click here.