Myopia is increasingly prevalent among younger patients, impacting nearly one-third of children and adolescents worldwide,1 and early intervention is critical in preventing high myopia and related ocular complications. Orthokeratology (ortho-k) lenses offer both refractive correction and effective myopia control via peripheral myopic defocus. This case report highlights the importance of technology in lens design as well as in the ongoing monitoring of pediatric myopia.
Case Description
A 10-year-old male patient presented to our clinic with symptoms of blurry distance vision, especially in the classroom and during sports. His unaided distance visual acuity was 20/100 in both eyes. Manifest refraction revealed:
- OD: -3.50 -1.25 x 180
- OS: -3.75 -1.00 x 175
Cycloplegic autorefraction confirmed these findings. The patient had no ocular history, but both parents had high myopia. Early and effective myopia control was considered essential given this risk profile.
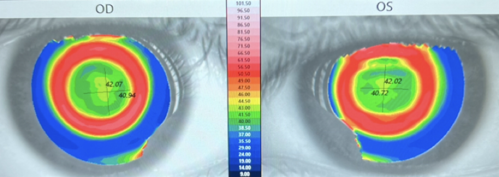
Corneal topography, elevation maps, keratometry, and axial length were all measured using the Myopia Expert 700 (Essilor) optical biometer, which integrates key biometric data for comprehensive myopia management. Topography confirmed symmetric with-the-rule astigmatism.
The elevation data allowed for precise quantification of sagittal height differences between the 2 principal meridians. In this case, the difference exceeded 30 µm, confirming the need for a toric stabilization zone design in the ortho-k lens. This helped optimize centration, comfort, and treatment zone stability. Axial lengths were above the pediatric age norm, further reinforcing the need for intervention.
The patient and family chose ortho-k treatment due to its dual function: correcting vision and controlling myopia progression. The Stellest (Essilor Contact lens) ortho-k toric lens design was empirically calculated using elevation data from the topographic maps.
Lens adaptation was smooth, with the patient achieving 20/25 uncorrected visual acuity within the first week and 20/20 by the 1-month follow-up. The lens showed excellent centration on subsequent topographic mapping with no corneal staining (see Figure 1).
At the 6-month review, repeat biometry scans showed minimal axial elongation:
- OD: +0.06 mm
- OS: +0.05 mm
These results suggested a slower than expected progression trajectory, and the patient remained compliant and highly satisfied with the treatment.
Discussion
This case demonstrates the value of using high-resolution elevation and axial length data to guide ortho-k lens design and treatment in complex cases. The ability to measure corneal elevation differentials provided the data needed to select the appropriate amount of toricity on the back surface of the lens, leading to optimal fit and efficacy.
In addition, the built-in biometer allows the clinician to confidently monitor for excessive myopic progression and is essential to any myopia management practice. By integrating axial length biometry, corneal topography, keratometry, and elevation mapping into a single platform, it allows clinicians to diagnose, monitor, and customize treatment with exceptional precision.
This level of data-driven care is essential for tracking progression, optimizing lens design—particularly in complex cases with astigmatism—and demonstrating treatment efficacy to patients and their families. As myopia rates rise globally, eye care clinicians who incorporate such advanced instrumentation ensure that their practices remain at the forefront of clinical care and patient outcomes.
References
- Liang J, Pu Y, Chen J, Liu M, Ouyang B, Jin Z, Ge W, Wu Z, Yang X, Qin C, Wang C, Huang S, Jiang N, Hu L, Zhang Y, Gui Z, Pu X, Huang S, Chen Y. Global prevalence, trend and projection of myopia in children and adolescents from 1990 to 2050: a comprehensive systematic review and meta-analysis. Br J Ophthalmol. 2025 Feb 24;109(3):362-371. doi: 10.1136/bjo-2024-325427. PMID: 39317432.
To hear Dr. Biondo discuss this case, click here.